How AI Can Optimize Accounts Receivable Management

Collaborating with professional billing consultants or joining group purchasing organizations (GPOs) may also provide leverage in negotiations. Consider outsourcing billing functions to third-party vendors or billing companies to alleviate staffing shortages and ensure timely claim processing, like Transcure. They have 1100+ qualified billers and coders to meet the needs of both small and large practices. Investing in ongoing staff training and education on regulatory changes, as well as implementing robust compliance management systems, can help ensure adherence to industry standards. Additionally, partnering with experienced billing and coding vendors who stay updated on regulatory changes can provide added assurance of compliance. Accounts receivable management plays a critical role in maintaining the cash flow of your practice and building a financially thriving and strong practice.

Why Charge Capture is Critical for Hospital AR
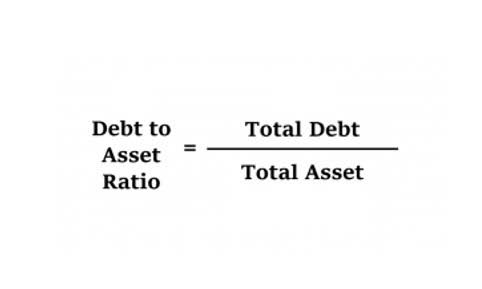
With unique challenges such as insurance involvement and high deductibles, healthcare organizations must implement strategic practices to mitigate risks and maximize revenue. Account Receivable refers accounts receivable in healthcare to the cost of a particular service provided for a patient by any medical coding services or provider billed during medical billing. A strong account receivable (AR) process is critical for organizations in every sector, including healthcare.
- Negotiating favorable reimbursement rates with insurance companies can be challenging for healthcare providers, especially smaller practices with limited bargaining power.
- This comprehensive guide aims to navigate the intricate maze of AR, showcasing its pivotal role in healthcare, and illustrating how adept management can catalyze a significant transformation in the industry.
- Clearly communicate payment policies during the patient registration process and provide flexible payment plans for convenience.
- Powerful AR automation tools include complex data extraction features that enable medical companies to work with complicated Explanation of Benefit (EOB) forms.
How should healthcare teams monitor AR performance effectively?
Nick has managed billing & coding departments overseeing all functions & responsibilities including developing programs to optimize healthcare center’s RCM functions to improve overall financial performance. Nick has worked with Hospitals, Provider Groups, FQHCs, and Surgery Centers of all specialty types and sizes to ensure performance KPIs are achieved and maintained to meet monthly & annual goals. Nick effectively communicates with C-level executives and Revenue Cycle Directors to achieve both short-term and long-term objectives to meet the needs of AnnexMed’s clients. Inadequate billing staff with insufficient training can be disastrous for the revenue Statement of Comprehensive Income cycle of a health organization. Implement standardized protocols for collecting and verifying patient information during registration or intake processes, including insurance verification and demographic updates. Leverage EHR systems to capture and store patient information accurately, reducing the likelihood of data entry errors and ensuring consistency across documentation.
- It defines the unreceived but recognized revenue and is recorded as a current asset in the statement of financial position.
- Finally, the organization should be prepared to clarify whether the assistance being sought is a one-time, periodic or ongoing transaction.
- This transparency enhances patient satisfaction and trust in the healthcare provider.
- First, providers must submit accurate bills to insurance companies and patients.
The Growing Challenge of Claim Denials and Delayed Reimbursement on Healthcare Providers
Our effective denial prevention strategy and dedicated denials team can help your organization increase payment recovery. This is done by identifying the root cause of denials, reworking the denials, writing appeals if necessary and CARES Act resubmitting claims. Insurance companies often take weeks or even months to process claims, creating cash flow gaps that can strain healthcare organizations’ budgets. Delayed reimbursements can severely impact financial planning and operational continuity.
- One of the most difficult challenges for any healthcare organization is keeping a stable cash flow.
- Audit is crucial to detect potential risks and problems in the Revenue Cycle Management.
- Serdeen’s dynamic leadership, coupled with his diverse experience and personal interests, makes him a valuable asset both within and outside the corporate arena.
- Streamlined efficiency in accounts receivable management is pivotal for the financial health of medical billing operations.
- His commitment to precision and a client-centric approach ensures that every account is managed efficiently, delivering positive outcomes for both the organization and its partners.
- This practice not only improves cash flow but also minimizes the risk of unpaid balances and bad debts.
A report from the Ponemon Institute estimates healthcare organizations average $3.7 million in lost revenue per data breach, but a report from Accenture estimates the cost could be as high as $113 million. According to Kristina B. Ziehler, MPH, is assistant director, data solutions, for the Medical Group Management Association (MGMA). Kristina says “Let’s start with the percentage of accounts receivable (A/R) in each aging category. When reviewing this particular benchmark, your company wants the majority to be in the days in A/R category. When benchmarking days in A/R, you want to compare yourself to the mean (or average). Based on this, your billing office would want to look at ways to improve their 0-30 days in A/R benchmark since it is lower than the MGMA benchmark.
